A new report out by North Carolina's Broadband and Infrastructure Office looks at the ways that broadband and telehealth can solve some of the disparities that disproportionately affect tens of thousands of its citizens living in the western fifth of the state. These “coal-impacted communities,” it argues, would benefit greatly across a host of interventions which would be facilitated by investment in wireline broadband infrastructure, technical assistance, and digital literacy programs. If implemented, they would increase access to medical doctors and mental health professionals for all North Carolinians, eliminate barriers related to transportation, reduce state healthcare costs, increase the speed of intervention and reduce the time to diagnosis, and eliminate unnecessary hospital and emergency room admissions.
Healthcare in the High Country
"Carolina Crosscut: Broadband and Telehealth in North Carolina's Appalchain Coal-Impacted Communities" [pdf] comes out of a $100,000 Appalachian Regional Commission grant given to the Office of Broadband Infrastructure and the Office of Rural Development for two purposes: to figure out broadband availability and adoption as they relate to health disparities across the twenty-county region clustered along the state’s western border, and to map assets and come up with specific policy recommendations for state agencies and lawmakers.
These are North Carolina’s “coal-impacted” communities, which the report defines as those which exhibit a “generational dependence on coal extraction and related supply chains [which] has resulted in personal and community economic devastation.” To be clear and despite its title, the framing here is economic, and not based on the adverse health effects of working in coal extraction. It should also be noted that the economic impact described in the report surely extended beyond the twenty counties at the center of the study.
Carolina Crosscut collects and collates a plethora of data that should be useful to any number of groups moving forward. It maps broadband access, adoption, and speeds at the census tract level against a cluster of health and mental health variables as well as existing assets and interventions at hospitals in the group of counties to determine what would happen if fast, affordable, reliable Internet were to become universally available. According to the report:
As a whole, residents in North Carolina’s Appalachian coal-impacted communities are sicker, have access to fewer health care providers, have less broadband available to them, adopt broadband at lower rates, and do not have the computers or skills needed to use telehealth services.
It drills down to what it says are the collection of health disparities that tell us most about these twenty counties characterized as the most rural, mountainous, and least connected in the state, including death rates for diabetes, stroke, and cardiovascular disease, the ratio of residents to health care providers for dentistry, mental health, and primary care, the number of mentally unhealthy days reported in the past month, and the sum of accidental opioid deaths from 2009-2018. The study takes particular aim at solving these problems via telehealth programs at 156 of what it defines as “safety net” sites — hospitals and clinics which don’t turn people away for lack of ability to pay, and which as a result treat the most economically vulnerable groups within their communities.
We Can Do Better
The findings and recommendations presented in the study are troubling (often dramatically so), but not world-shattering, and that’s a good thing: they suggest the state can solve them with the right investments, technical assistance, and oversight without having to develop new policy solutions out of whole cloth. Further, the report concludes, there are significant savings to be realized and economic potential to be unlocked in doing so. Read the report for the comprehensive collection of findings, but some of the most important are below:
- Local needs take primacy above all else, and so local leaders need to be given the tools to meet challenges and take advantage of assets.
- The absence of a cohesive approach means illness costs the state money on both ends: sick people don’t work, but telehealth initiatives can also reduce the cost of delivering medicine and services.
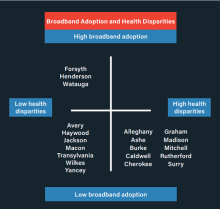
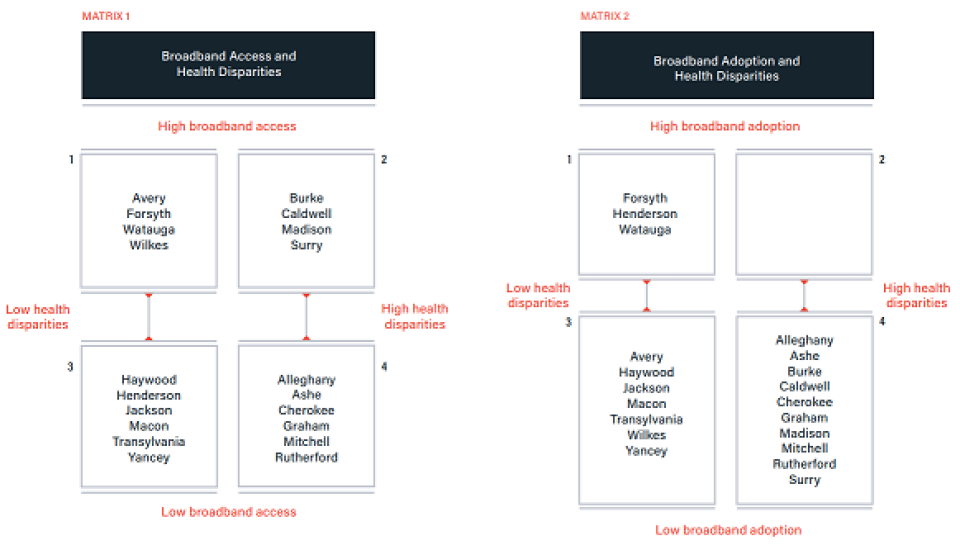
- Not one of the twenty counties in the study showed both high broadband adoption rates and health disparities. Thus, while broadband availability necessarily takes place before adoption, the latter is key.
- In most of these communities, both access and adoption are low, and in many cases much lower than the state average.
- North Carolina does not have a shortage of physicians, just an uneven distribution of them, but safety net sites do not feel prepared to establish telehealth programs. If the state could connect its medical experts to its populations in need, everyone wins.
- At minimum broadband access speeds of 25 Megabits per second (Mbps) download and 3 Mbps upload — which the report calls the minimum for delivering telehealth services — an estimated 71,637 households in the 20 county-region are unserved. This accounts for 30 percent of the total estimated number of unserved households (239,945) statewide. Thus, even if telehealth programs were abundant and mature today, these households would not be able to take advantage. Solving this gap remains one of the most crucial barriers.
- Computer access contributes mightily to the digital divide: 91,420 households in the study area do not have computers, and rely on oft-capped mobile connections for access.
Main recommendations
The report details seven areas the state can improve and address the above disparities:
- Programs and health interventions should be tailored to each community’s specific needs.
- Develop a cohesive state policy to enable telehealth expansion. Through the Office of Rural Health, the state should provide technical assistance to safety net sites to support telehealth Implementation.
- The state, federal government, partners and stakeholders should dedicate resources to increase broadband availability to unserved households in the coal-impacted counties.
- The state, partners and stakeholders should implement innovative and comprehensive broadband adoption and digital inclusion programs.
- Encourage safety net sites to evaluate their broadband subscription before launching telehealth programs.
- Entrepreneurial support organizations should provide intentional support for entrepreneurs who desire to launch digital health startups in the coal-impacted counties.
Other recommendations
Carolina Crosscut offers some additional recommendations as well, including expanding the state's Growing Rural Economies with Access to Technology (GREAT) program and increasing the threshold for "unserved" from its official current metric of 10/1 Mbps to a connection capable of supporting telehealth interventions, lest those communities will be left behind. The report calls at the national level for an expansion of the Federal Communication Commission's Health Care Connect Fund. The report conlcudes:
[C]lear, bold and swift actions from state and local leaders are necessary to ensure North Carolina’s Appalachian coal-impacted communities do not remain sicker, more economically distressed, and without the digital infrastructure necessary to flourish in the 21st century.
In addition, the project team created three dashboards designed to assist decisionmakers and stakeholders as they view the region’s broadband and health disparities. For more, read the whole report [pdf], which includes five site case studies on sites with specific interventions to learn from (in Mount Olive, Marion, Asheville, Greenville, and Ahoskie) as well as a more detail on each county in the appendix. North Carolina has ambitious broadband plans, and this report offers some practical ways to meet them where North Carolinians currently live.
Image by David Mark from Pixabay